Focus on Broadband and Chronic Disease
Chronic diseases such as diabetes, heart disease, cancer, and obesity are the leading cause of illness, disability, and death in America (opens new window). They are also key factors impacting the United States’ annual health care costs, estimated at $4.5 trillion (opens new window).
The Key Role of Broadband Connectivity
Telehealth and other broadband-enabled solutions and technologies can play an important role in chronic disease prevention and management, leading to improved (opens new window) patient outcomes, access to care (opens new window), and cost savings. Previous research (opens new window) by the Connect2Health Task Force has shown that counties with higher levels of broadband connectivity—i.e., access and, more significantly, adoption and use—had lower diabetes prevalence, suggesting that there is a relationship between broadband connectivity and chronic disease. In fact, meta-analyses (opens new window) have shown that telehealth and other digital health innovations are effective (opens new window) for prevention and management of numerous chronic disease conditions. For example:
- Wearable devices, like fitness trackers, smartwatches, and biosensors, can monitor and share with health care providers physiological metrics (e.g., heart rate, blood sugar levels, blood pressure). Chronic disease patients and health care providers can detect deviations from normal patterns, allowing for early detection of potential health issues. Remote patient monitoring has helped improve blood sugar (glucose) levels (opens new window), lower blood pressure (opens new window), reduce hospital readmission rates (opens new window), and save money (opens new window).
- Broadband-enabled artificial intelligence and machine learning technologies leverage large datasets to identify patterns, predict health risks, and assist with decision-making. Algorithms can assess an individual's risk of developing certain chronic conditions (opens new window). Health care providers can recommend tailored lifestyle interventions to those individuals with higher chronic disease risk.
- Mobile health (mHealth) applications enable individuals to track physical activity, monitor diet, manage medications, and access personalized health information, supporting behavioral changes critical for chronic disease prevention. Poor diet, insufficient physical activity, and smoking contribute to conditions like diabetes, cancer, and heart disease. MHealth tools help users set tailored goals, track progress, access educational resources, and receive reminders for healthy choices. The Community Preventive Services Task Force recommends (opens new window) mHealth interventions (opens new window) for quitting tobacco and electronic screening to reduce heavy drinking (opens new window). Research shows digitization moderates (opens new window) the link between chronic disease and physical activity in middle-aged and older adults. MHealth interventions also improve dietary outcomes (opens new window), including increased fruit and vegetable consumption, reduced sodium intake, and weight loss (opens new window).
- Telemedicine platforms enable remote consultations and medical advice via video conferencing, telephone, or chat. Telemedicine can increase access to healthcare for patients in rural (opens new window) or underserved areas. Telehealth has been used effectively to manage chronic disease conditions (opens new window).
- The internet has become a primary resource (opens new window) for health-related information, and the Internet facilitates (opens new window) ongoing communication outside clinic visits essential for chronic disease management.
While these connected health interventions have significant potential, broadband connectivity is a baseline requirement. For example, patients with higher download and upload speed (≥100/≥100 Mbps) versus lower ( ≤Mbps/ ≤3 Mbps) broadband access use video telehealth more frequently (opens new window). As another example, lack of broadband connectivity can inhibit patients' use of remote monitoring services (opens new window). According to recent data, 28% of people living in rural areas and 23% of people living on tribal lands (opens new window) do not have access to adequate broadband. Internet access gaps (opens new window) can affect the use of connected health in rural and other vulnerable populations.
Background on Chronic Disease in the U.S.
Chronic diseases are defined (opens new window) broadly as health conditions that last one year or more, require ongoing medical attention, and limit activities of daily living. For example:
- Cardiovascular disease is the leading cause of mortality in the United States, and trends are increasing. Heart disease and stroke could affect 60% of U.S. adults by 2050 (opens new window), with annual health care costs projected to almost quadruple (opens new window), from $393 billion currently to $1490 billion by 2050.
- In 2021, 1,777,566 new cancer cases were reported; and in 2022, over 600,000 people died (opens new window) of cancer in the United States. By 2040, new cancer cases are expected to increase (opens new window) to 29.9 million per year, and the number of cancer-related deaths is expected to increase to 15.3 million per year.
- About 10% of Americans have diabetes (opens new window), and more children and young adults are developing diabetes than in the past. The diabetes rate is expected to rise to 26.8% (opens new window) of the population by 2050, and the population-level health care cost attributable to diabetes is projected to increase from $186 billion in 2020 to $765 billion in 2050 (opens new window).
- Obesity rates are expected to climb from 43.1% to 60.6% of the population by 2050 (opens new window), and obesity is expected to affect the health condition of a third of all children by 2050, up from 20% in 2020.
Smoking, poor nutrition, physical inactivity, and excessive alcohol use cause most chronic diseases. Cigarette smoking (opens new window) causes cancer, heart disease, stroke, lung diseases, and diabetes and leads to more than 480,000 deaths each year in the United States. Poor nutrition (opens new window) and physical inactivity (opens new window) are significant risk factors for obesity, type 2 diabetes, heart disease, stroke, some types of cancer, and depression. Meanwhile, excessive alcohol use (opens new window) is associated with high blood pressure, heart disease, stroke, liver disease, and some types of cancer.
Some groups are impacted more strongly by chronic disease (opens new window) than others because of the conditions in which they are born, grow, work, and live that limit their ability to make healthy choices. These factors include, but are not limited to, poverty, unsafe or unhealthy environments, unsafe or unaffordable housing, food insecurity, and lack of access to quality education and jobs. The FCC’s Connect2HealthFCC Task Force’s Chronic Disease Conceptual Framework provided below summarizes these conditions in Demographic Factors, Community & Geographic Factors, Risk Factors, Access to Care, and Quality of Care. For instance:
- The location and quality of food retail options as well as the cost of healthy foods impact dietary patterns (opens new window), an important risk factor for chronic disease.
- Access to primary care physicians (opens new window) offers early chronic disease detection, treatment, management, as well as preventive care.
- Uninsured adults (opens new window) are less likely to receive preventive services for chronic conditions such as diabetes, cancer, and cardiovascular disease.
- Veterans (opens new window) have higher rates of chronic disease than the general population.
- Generally, people experiencing poverty (opens new window) are at higher risk for chronic disease.
Mapping the Intersection of Broadband and Chronic Disease
Since 2017, the Mapping Broadband Health in America platform has allowed users to view the intersection of broadband connectivity and chronic disease outcomes, access to care indicators, chronic disease risk factors, social and economic factors, and physical environment factors. The 2025 release includes an updated conceptual model (shown below) to outline the complex intersection of broadband and chronic disease. Mapping Broadband Health in America platform users can now:
- Ask questions like: What is the status of Internet connectivity in areas where heart disease, cancer, diabetes or poor/fair health prevalence are highest?
- Generate actionable insights for policies and programs about how broadband connectivity can be leveraged to improve chronic disease outcomes and identify health disparities.
- Display selected data on broadband connectivity (e.g., fixed and mobile access, Internet adoption, rural access, device ownership) and chronic disease outcomes with key variables to generate customized maps at the state and county levels.
- View heart disease, cancer, or diabetes rates filtered by demographics, social and economic factors, race/ethnicity, physician access, and rurality to visualize patterns, possible disparity issues, and locations where broadband-enabled interventions are most impactful.
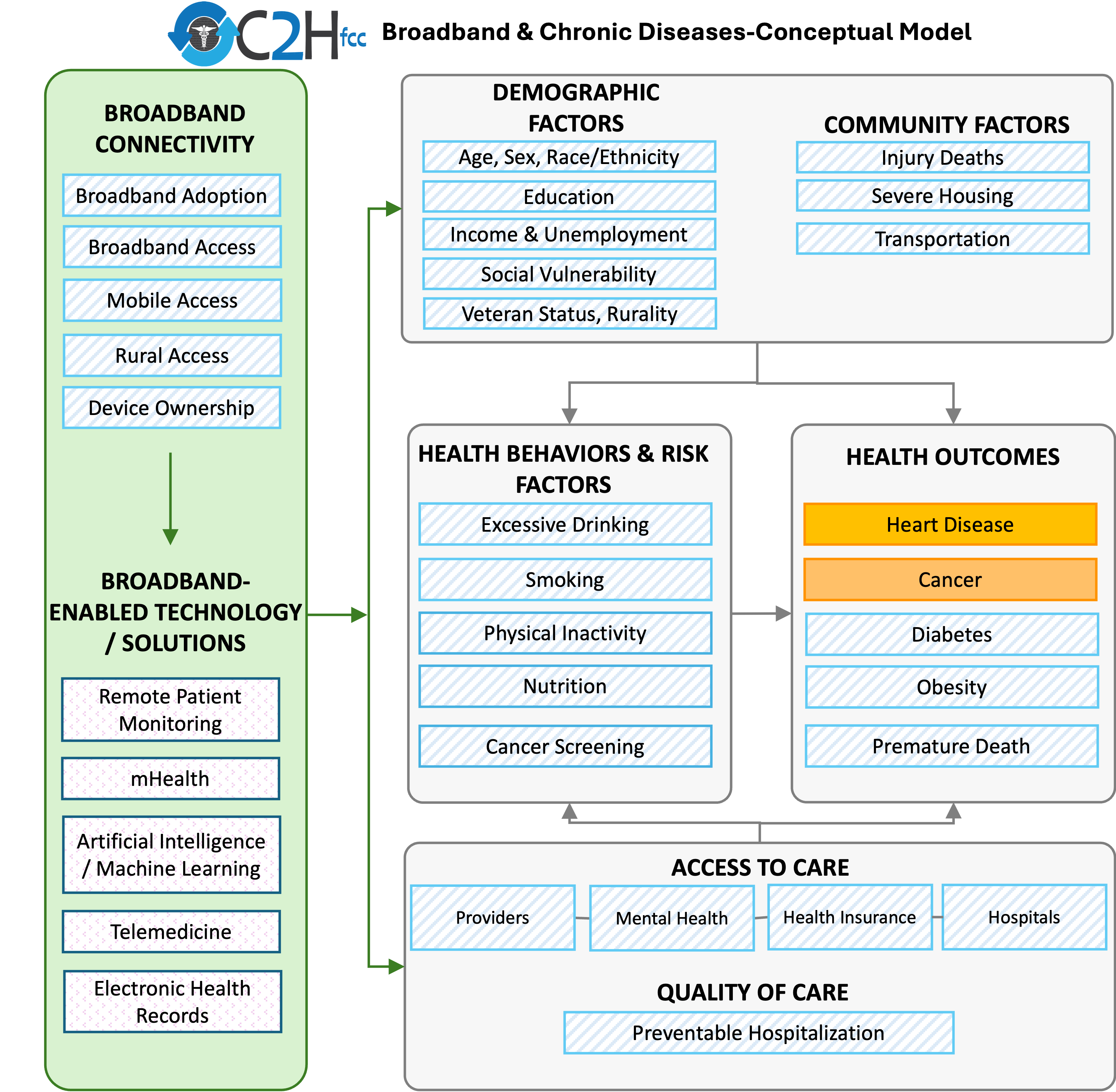
KEY: Orange represents the most recently added items from the 2025 release; blue diagonal lines denote items included in previous releases; and pink dots represent technology solutions that use broadband connectivity and can improve chronic disease outcomes (note that the platform does not include data for this set of variables).
The Task Force identified key broadband connectivity factors that enable the use of digital solutions to improve chronic disease outcomes.
- Broadband Adoption: Based on 2019-2023 Census American Community Survey data, on average approximately 75% of households in a county report subscribing to high-speed Internet (e.g., cable, DSL, fiber optic).
- Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average approximately 92% of individuals in a county have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Mobile Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 97% of individuals in a county have access to outdoor stationary mobile 5G-NR service at 35/3 Mbps or higher advertised speeds.
- Rural Fixed Broadband Access: Based on 2024 FCC Broadband Data Collection (BDC) data, on average around 90% of those living in rural census blocks have access to fixed terrestrial broadband service at 100/20 Mbps or higher advertised speeds.
- Device Ownership: Based on 2019-2023 Census American Community Survey data, on average approximately 6% of households in a county report having no computing devices. Access to digital devices (opens new window) is associated with preferring telehealth appointments over in-person visits.
- Funding: The FCC's Rural Health Care Program provides funding to eligible healthcare providers for telecommunications and broadband services necessary for the provision of health care. Over 2900 counties have received some level of funding between 2019 and 2024.
The Task Force identified relevant demographic factors that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The DEMOGRAPHIC FACTORS box of the framework includes nine measures:
- Age: Almost a quarter of the U.S. population is expected to be 65 or older by 2060 (opens new window), and aging increases the risk of chronic disease. The majority of the adult population 50 years and older, across all races, will have at least one chronic disease by 2050 (opens new window), with the majority between the ages of 60 to 79 years.
- Sex: Women are more likely than men to have multiple chronic conditions (opens new window) at the same time and more likely to have certain chronic conditions, such as Alzheimer’s disease and depression (opens new window).
- Race & Ethnicity: Chronic disease prevalence varies by race (opens new window). Black, Hispanic, and American Indian or Alaska Native (AIAN) adults are more likely to have diabetes than White adults. AIAN adults are also more likely to have had a heart attack or heart disease than White adults, while rates for Black, Hispanic and Asian adults are lower than White adults. White adults have lower rates of asthma than Black and AIAN adults but higher rates than Hispanic and Asian adults.
- Education: In the southeastern region of the U.S., areas with low educational attainment have the highest rates of chronic disease (opens new window).
- Median Household Income: Residents of impoverished communities are at increased risk for chronic disease (opens new window).
- Unemployment: Unemployment is associated with increased risk of developing chronic disease, including stroke, heart attacks, heart disease, and arthritis (opens new window).
- Social Vulnerability: Social Vulnerability is a composite measure based on 16 demographic factors collected in the American Community Survey, including poverty, unemployment, housing cost burden, education, health insurance, age, disability status, single-parent households, English language proficiency, racial and ethnic minority status, housing type and transportation. Some chronic diseases are associated with multiple Social Vulnerability factors. For example, chronic obstructive pulmonary disease (COPD) prevalence at the county level is strongly associated with disability, single-parent households, and socioeconomic factors (opens new window) of Social Vulnerability.
- Veteran Prevalence: Among adults aged 25 and over, the prevalence of multiple chronic conditions is higher among veterans (opens new window) than non-veterans. Obesity, diabetes, heart disease, stroke, chronic obstructive pulmonary disease (COPD), and chronic kidney disease are all more prevalent (opens new window) among veterans.
- Rurality: Rural residents have higher prevalence of multiple chronic conditions (opens new window) and are more likely than urban residents to die prematurely of heart disease, cancer, chronic lung disease, and stroke (opens new window).
The Task force identified relevant community factors that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The COMMUNITY FACTORS box of the framework includes three measures:
- Injury Deaths: Falls are a major cause of unintentional injury death (opens new window), and common chronic conditions such as arthritis, stroke, diabetes, dementia, and poor vision can increase the risk of falling (opens new window).
- Severe Housing: Housing instability is associated with higher prevalence of obesity, hypertension, diabetes, and cardiovascular disease (opens new window). Homeowners report , lower prevalence of multiple chronic conditions (opens new window), including angina, diabetes, asthma, stroke, and kidney disease.
-
Transportation:
Transportation barriers to health care have a
disproportionate effect (opens new window)
on individuals with chronic diseases, preventing them from attending medical appointments or traveling to pharmacies.
Some evidence suggests that providing transportation in combination with other tailored services can improve health outcomes (opens new window)
for patients with chronic diseases.
- Distance to emergency room: Median distance in miles to the nearest emergency department, calculated using population weighted tract centroids in the county.
- Percent of households with no vehicle: Percent of housing units with no vehicle available.
The Task Force identified relevant health behaviors and risk factors that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The HEALTH BEHAVIORS & RISK FACTORS box of the framework includes five measures:
- Excessive Drinking: Excessive drinking is associated with increased prevalence of chronic diseases (opens new window) such as high blood pressure, heart disease, stroke, liver disease, and dementia (opens new window).
- Smoking: Smoking is the leading preventable cause of death, disability, and disease in the U.S. Smoking causes heart disease, stroke, lung disease, diabetes, and other chronic diseases (opens new window).
- Physical Inactivity: Physical inactivity is a risk factor for heart disease, diabetes, and obesity (opens new window). Only 1 in 4 adults and 1 in 6 young people get the recommended amount of physical activity (opens new window).
- Food Insecurity/nutrition: Food insecurity is associated with multiple chronic health conditions (opens new window), including diabetes, hypertension, heart disease, chronic kidney disease, and depression. Individuals with chronic diseases are also more likely to lack the transportation and income (opens new window) necessary to obtain healthy food.
- Cancer Screening: Cancer screening leads to earlier detection and improved cancer outcomes (opens new window). The platform now includes the mammography screening prevalence data.
The Task Force identified relevant health outcomes that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The HEALTH OUTCOMES box of the framework includes five measures on the platform:
- Heart Disease: Heart disease variables include ischemic heart disease prevalence and mortality rate, cerebrovascular disease mortality rate, heart failure mortality rate, other cardiovascular disease mortality rate, stroke prevalence, high blood pressure prevalence, high cholesterol prevalence, and cardiovascular disease provider rate. Heart disease is the leading cause of death (opens new window) in the United States.
- Cancer: Cancer variables include incidence and mortality for all cancer, breast cancer, colon cancer, prostate cancer, and lung cancer as well as mammography screening, colorectal cancer screening, outpatient oncology providers, and number of hospitals with chemotherapy services / mammography services / oncology services. Cancer is the second leading cause of death (opens new window) in the United States.
- Diabetes: Diabetes shares risk factors with many other chronic diseases and is itself a risk factor for kidney disease, cardiovascular disease, and hypertension (opens new window).
- Obesity: The prevalence of obesity was over 40% (opens new window) among U.S. adults aged 20 and older between 2017 and 2020 and is increasing. Obesity contributes to multiple chronic diseases and is independently associated with cardiovascular disease (opens new window) and cardiovascular disease mortality.
- Premature Death: Three of the five leading causes of premature death in the U.S. from 2010-2022 were chronic diseases (opens new window): stroke, chronic lower respiratory disease, and heart disease. Variation in the rate of premature death (opens new window) due to noncommunicable chronic disease at the county level is associated with demographic composition, socioeconomic features, health care environment, and population health status.
The Task Force identified relevant access to care components that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The ACCESS TO CARE box of the framework includes eight measures:
- Access to Care
- Physician Access: Having a primary care provider is important for maintaining health and managing disease (opens new window).
- Dental Providers: Number of dentists. Untreated periodontitis (gum disease) can make other chronic conditions worse (opens new window). Evidence suggests that periodontal treatments (opens new window) can improve lung function in patients with chronic obstructive pulmonary disease (COPD), improve severity measures in patients with diabetes, and improve measures of inflammation in patients with cardiovascular disease.
- Mental Health Providers: Number of mental healthcare providers. In the U.S., 1 in 3 individuals lives in an area with a shortage of mental health providers (opens new window). Individuals with mental health conditions such as depression are at higher risk for developing certain chronic diseases (opens new window), including heart disease, diabetes, stroke, and Alzheimer’s disease. Chronic disease can also increase the likelihood of developing mental health conditions; Americans with diabetes are 2-3 times more likely to develop depression (opens new window).
- Access to Cancer Care: People living in rural areas tend to have limited access to cancer care (opens new window). Access to cancer care includes number of hospitals with mammography services, number of hospitals with chemotherapy services, number of hospitals with oncology, services, and outpatient oncology providers.
- Health Insurance:
Health insurance can help individuals with chronic diseases receive diagnosis and treatment. For example,
lack of health insurance is associated with delaying or avoiding care because of costs, including preventive care and services for chronic illnesses (opens new window).
Health insurance includes:
- Medicaid insurance: Percentage of population with any Medicaid/means-tested public health insurance coverage.
- Medicare insurance: Percentage of the population with Medicare health insurance coverage only.
- Private insurance: Percentage of the population with private health insurance coverage.
- Health insurance: Percent of persons under 65 with medical insurance.
The Task Force identified relevant quality of care components that influence chronic disease outcomes and where broadband-enabled interventions might help bridge the gaps. The QUALITY OF CARE box of the framework includes one measure:
- Preventable Hospitalization: Rate of hospital stays for ambulatory-care sensitive conditions per 100,000 Medicare enrollees (age-adjusted). Women, Black and American Indian/Alaska Native adults, adults ages 65 and older, and adults from lower-incomecommunities are all more likely to experience preventable hospitalization (opens new window). These populations are also more likely to have chronic diseases such as diabetes, heart disease, and Alzheimer’s disease.
Future Work
The Mapping Broadband Health in America platform is a foundational tool for understanding the intersection of broadband and health, giving policymakers, researchers, advocacy groups, broadband service providers, innovators, and other interested parties a concrete path to a more connected and healthier future for all Americans.
The Task Force will continue to refine the conceptual approach going forward and welcomes comments and suggestions from interested parties via e-mail to engageC2H@fcc.gov(opens new browser window with "Mapping" in the subject line).